A 66- year- old male presented with complaints of recurrent jaundice, pain in abdomen and fever
- A 66-year-old male presented with complaints of recurrent jaundice, pain in the abdomen, and fever
- No history of significant weight loss
- No other significant complaint
FINDINGS
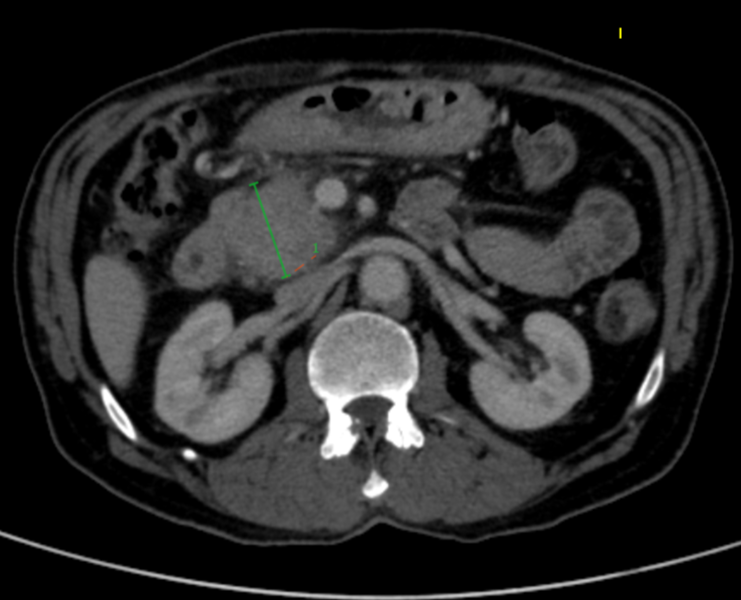
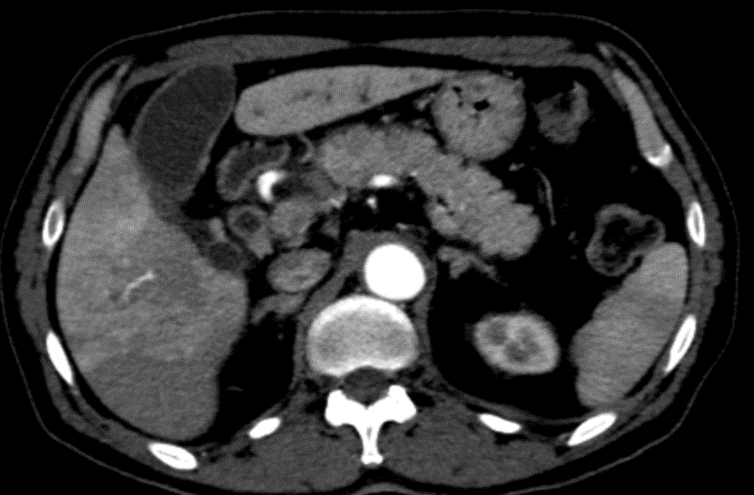
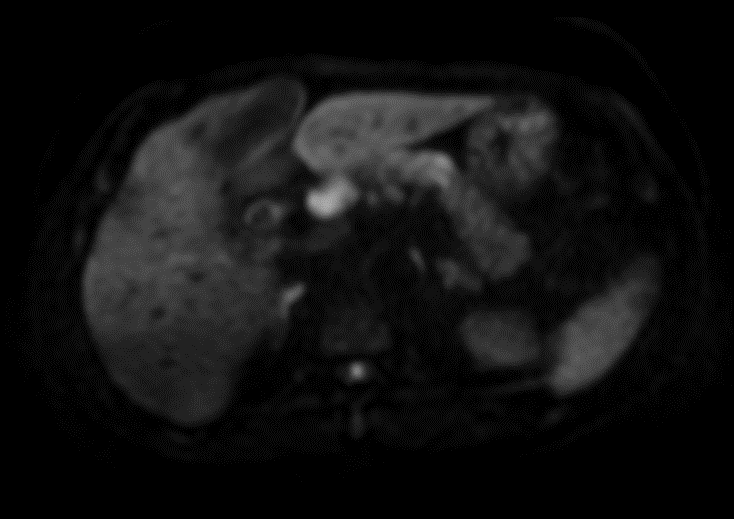
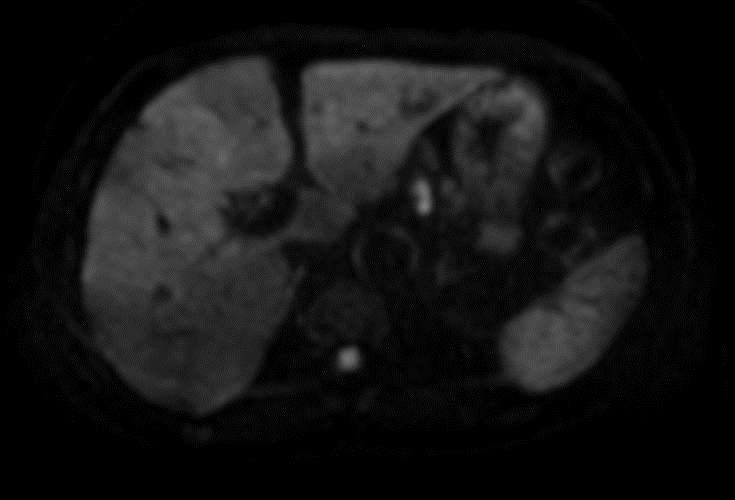
- Scattered segmental biliary dilatation in both lobes, more pronounced in segments 2 & 3 with mild thickening and enhancement of bile duct walls on post-contrast images (blue arrows in fig.1&2). A 16x11mm simple cyst was noted in segment 6 of the liver(orange arrow in Fig. 1)
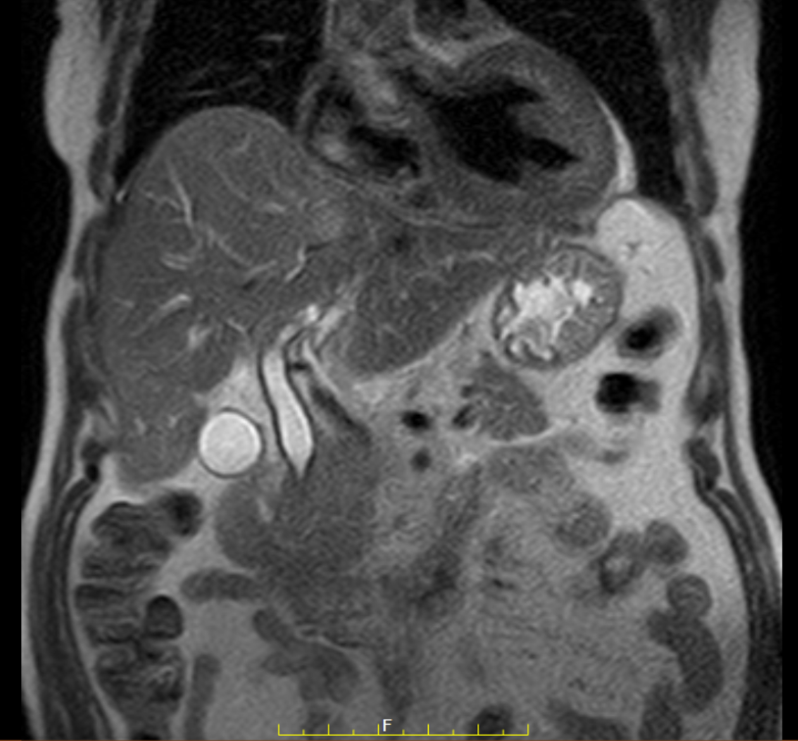
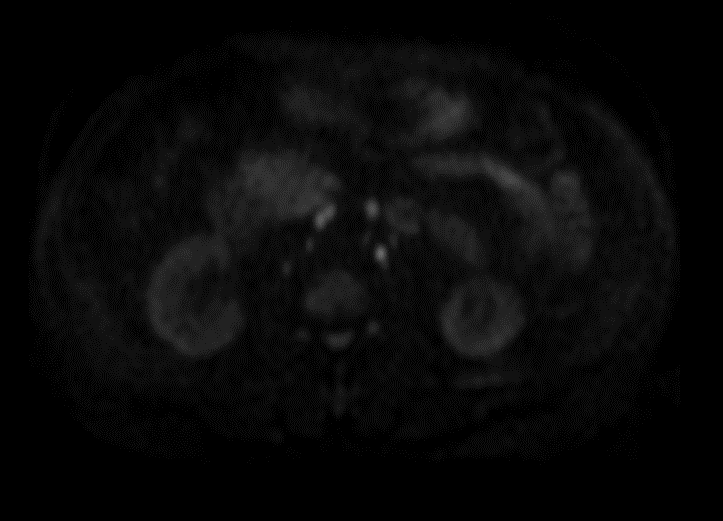
- Circumferential wall thickening showing enhancement on post-contrast images, involving the extra-hepatic bile ducts(white arrow in fig.4) , common bile duct (green arrow in fig.2&4), and cystic duct(orange arrow in fig.3) . Mild dilatation of extra-hepatic(white arrow in fig.4) and common bile duct seen(green arrow in fig.2&4) -11mm diameter.
- Patchy differential enhancement of liver parenchyma(white arrowheads in fig. 1&2)-likely represents Transient hepatic attenuation differences(THAD).
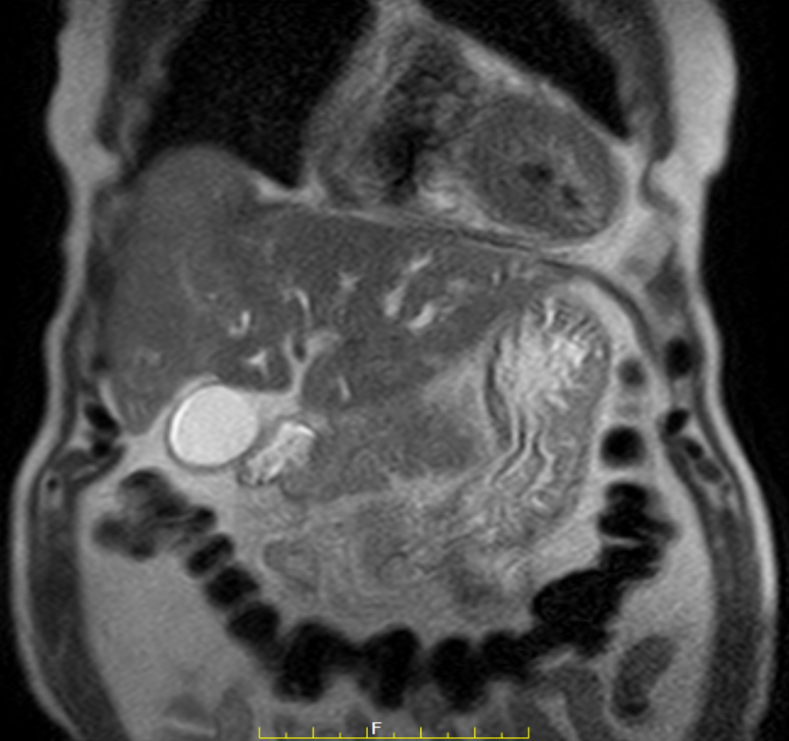
- Long segment smooth narrowing of intra-pancreatic portion of distal common bile duct with enhancing walls(red arrow in fig.5).
- Bulky head of the pancreas(green line measurement in Fig. 6) with mild adjacent fat strandings. The Main pancreatic duct(MPD) is normal(white arrow in Fig. 7). The body and tail of the pancreas are unremarkable(orange arrow in Fig. 8)
- Correlative MRI confirms the above findings of segmental biliary dilatation and dilatation of extra-hepatic (blue arrows in fig. 9&10) and common bile duct (green arrow in fig.9) with smooth narrowing of an intra-pancreatic portion of the distal common bile duct(red arrow in fig. 9).
- Note also made of abrupt narrowing at the junction of segment 2 and 3 ducts-s/o fibrotic tissue/stricture (orange arrows in Fig. 10).
- Restricted diffusion in the thickened bile duct walls(green arrows in Fig. 11&12)
- The note is also made of restricted diffusion in the head of the pancreas(red arrows in Fig. 13&14)
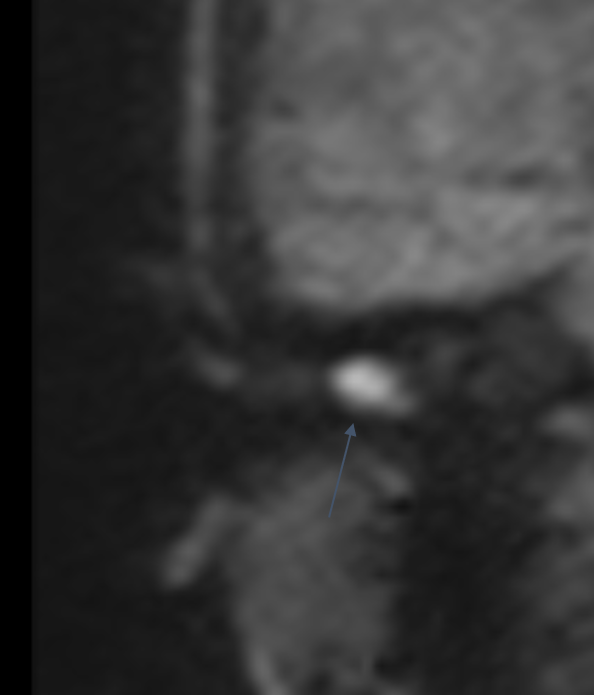
- An enlarged periportal node (~18mm on the short axis) was noted with restricted diffusion(red arrow in Fig. 15).
- Multiple sub-centimetric perigastric, peripancreatic, and upper retroperitoneal nodes with restricted diffusion(green arrows in Fig. 16&17).
DIAGNOSIS:
IGG4 related disease presenting as Sclerosing cholangitis ,Focal autoimmune pancreatitis and periportal, peripancreatic and upper retroperitoneal lymphadenopathy
DISCUSSION:
- Immunoglobulin G4 (IgG4)–related disease is a relatively recently proposed clinical-pathologic entity that is characterized by fibro-inflammatory lesions rich in IgG4-positive plasma cells and, often but not always, elevated serum IgG4 concentrations.
- IgG4-related disease was recognized as a systemic disease in 2003, when extrapancreatic manifestations were identified in patients with autoimmune pancreatitis. Since then, the disease has been reported as affecting virtually every organ system and has been identified in the biliary tree, salivary and lacrimal glands, periorbital tissues, lungs, lymph nodes, thyroid gland, kidneys, prostate gland, testicles, breasts, and pituitary gland.
- Its pathogenesis is poorly understood, but findings are consistent with both an autoimmune and an allergic disorder. Although definitive diagnosis requires histopathologic analysis, imaging plays an important role in demonstrating infiltration and enlargement of involved organs.
- The common features include infiltration by IgG4-positive plasma cells and lymphocytes with associated fibrosis, producing tumefactive lesions in one or more organs or organ systems.
- The pancreas is the most commonly affected organ in IgG4-related disease
- Many different terms have been used in the literature to describe IgG4-related disease, including IgG4-related sclerosing disease, IgG4-related systemic disease, IgG4-related autoimmune disease, and systemic IgG4-related plasmacytic syndrome . Because the fibrosis is characteristically found in some organs but seldom in others, and because the disease may be systemic or may affect only a single organ, terms like sclerosing or systemic are not precise for referring to this spectrum of disease. A panel of Japanese investigators recently reached a consensus to simply use the term IgG4-related disease.
- The Japanese group proposed three major diagnostic criteria for practical use: (a) clinical examination showing characteristic diffuse or localized swelling or masses in one or more organs; (b) hematologic examination showing elevated serum IgG4 concentrations (≥135 mg/dL); and (c) histopathologic examination showing marked lymphoplasmacytic infiltration and storiform fibrosis, as well as organ infiltration by IgG4-positive plasma cells
IgG4-related Autoimmune Pancreatitis
- There are two main recognized patterns of autoimmune pancreatitis: diffuse and focal.
- Diffuse disease is the more common pattern and is characterized by a uniformly enlarged pancreas with absence of pancreatic clefts. The pancreas has a sharp margin and loss of lobular contours, resulting in a featureless sausagelike appearance.
- Focal disease is characterized by enlargement of the pancreatic head or, less frequently, the pancreatic body or tail, resulting in a masslike appearance. Focal disease accounts for approximately 33%–41% of all cases, and its radiologic appearance may be difficult to differentiate from that of pancreatic carcinoma
- The affected area of the pancreas in patients with autoimmune pancreatitis typically appears hypoechoic at ultrasonography (US),hypoattenuating at computed tomography (CT), mildly hyperintense at T2-weighted magnetic resonance (MR) imaging, and hypointense at T1-weighted MR imaging . Dynamic CT shows a distinctive delayed enhancement pattern due to the presence of parenchymal fibrosis
- The apparent diffusion coefficient(ADC) value of autoimmune pancreatitis was found to be significantly lower than that of pancreatic cancer because of the greater cellularity of the former condition
IgG4-related Sclerosing Cholangitis
- Aside from the pancreas, the bile ducts are the most commonly involved organ in IgG4-related disease; about 60%–80% of patients with type 1 autoimmune pancreatitis have involvement of the hepatobiliary tract.
- Both the intrahepatic and extrahepatic segments can be affected, producing dense bile duct infiltration by IgG4-positive plasma cells and extensive fibrosis. The result is focal or diffuse bile duct wall thickening, mostly associated with stenosis and upstream dilatation, findings that are readily depicted at ERCP and MR cholangiopancreatography.
- The most commonly involved segment is the intrapancreatic portion of the CBD, since most cases of IgG4-related sclerosing cholangitis are associated with autoimmune pancreatitis.
Salivary and Lacrimal Gland Involvement
- Patients present with either enlargement of the lacrimal and salivary glands (an entity previously known as Mikulicz disease) or chronic sclerosing sialadenitis of the submandibular glands (also known as Küttner tumor). In the past, both entities were erroneously viewed as subcategories of Sjögren syndrome; now, however, they are considered part of the spectrum of IgG4-related disease.
- At CT, the lesions in Mukulicz disease usually demonstrate homogeneous attenuation and enhancement . At MR imaging, they have relatively low signal intensity on T2-weighted images owing to fibrosis, and low signal intensity with homogeneous enhancement on T1-weighted images.
- Küttner tumor is a relatively uncommon cause of salivary gland enlargement and was originally described as a “hard swelling” of one or both submandibular glands.
Orbital Involvement
- Patients with IgG4-related ophthalmic disease primarily show involvement of the lacrimal gland. This IgG4-related dacryoadenitis is usually bilateral, and concurrent salivary gland enlargement (Mikulicz disease) is common.
- A substantial proportion of idiopathic orbital inflammations—also called orbital pseudotumors—are associated with IgG4-related disease.
- At CT, orbital pseudotumors show soft-tissue attenuation and homogeneous enhancement. At MR imaging, these pseudotumors demonstrate low signal intensity relative to brain on T2-weighted images and tend to appear hyperintense on diffusion-weighted images because of fibrosis.
IgG4-related Thyroiditis
- Two forms of thyroid involvement in IgG4-related disease have been described: Riedel thyroiditis and the fibrous variant of Hashimoto thyroiditis. Riedel thyroiditis is a rare form of chronic inflammatory process with extensive fibrosis, resulting in a rock-hard painless mass that involves the thyroid parenchyma and surrounding tissues.
- CT demonstrates either focal or diffuse low attenuation of the thyroid, with minimal contrast enhancement relative to normal thyroid tissue
IgG4-related Renal Disease
- Renal involvement may be present in up to 35% of patients with autoimmune pancreatitis . Five patterns of disease have been described: bilateral round or wedge-shaped peripheral cortical lesions (the most common), diffuse patchy involvement ,a rim of soft tissue around the kidney, bilateral nodules in the renal sinuses, and diffuse wall thickening of the renal pelvis.
- After contrast material administration, the renal lesions appear hypoattenuating relative to the normal renal cortex during the arterial phase, becoming isoattenuating relative to the surrounding parenchyma during later phases. At MR imaging, the lesions demonstrate low signal intensity on both T1- and T2-weighted images, with mild enhancement on T1-weighted images after contrast material administration
IgG4-related Lymphadenopathy
- Concomitant lymphadenopathy is often found in patients with IgG4-related disease. It sometimes represents the initial manifestation of the disease, but it is usually discovered at imaging of patients with known IgG4-related disease.
- Hilar lymphadenopathy was reported in 80% of patients with autoimmune pancreatitis . Other commonly involved lymph nodes include mediastinal , axillary, cervical, and intraabdominal nodes
- The lymph nodes in IgG4-related disease tend to be small (<2 cm), and patients experience no fever or weight loss.
IgG4-related Retroperitoneal Fibrosis
- Retroperitoneal fibrosis is a chronic inflammatory condition that may have many underlying causes, including infection, radiation therapy, drugs, malignant tumor, and trauma.
- At cross-sectional imaging, IgG4-related retroperitoneal fibrosis appears as a soft-tissue mass that covers the abdominal aorta and its branches or entraps the ureters, producing hydronephrosis and hydroureter
IgG4-related Sclerosing Mesenteritis
- Sclerosing (or retractile) mesenteritis is a rare chronic disorder that leads to localized or diffuse fibrosis and inflammation of the small bowel mesentery.
- A useful CT finding that helps differentiate IgG4-related mesenteritis from these entities is preservation of fat around the mesenteric vessels, a phenomenon that is referred to as the “fat ring sign”
IgG4-related Lung and Pleural Disease
- Hirano et al found lung involvement in 13% of patients with autoimmune pancreatitis. Four major types of IgG4-related pulmonary disease have been defined: (a) a type characterized by solid nodular or masslike lesions, (b) a type characterized by round ground-glass opacities, (c) alveolar interstitial disease, and (d) bronchovascular disease
Differential Diagnoses
- Pancreatic adenocarcinoma
- Primary sclerosing cholangitis
- Lymphoma
REFERENCES
- IgG4-related Disease from Head to Toe Anxo Martínez-de-Alegría, Sandra Baleato-González, Roberto García-Figueiras, Anaberta Bermúdez-Naveira, Ihab Abdulkader-Nallib, José A. Díaz-Peromingo, and Carmen Villalba-Martín RadioGraphics 2015 35:7, 2007-2025
- Hamano H, Kawa S, Horiuchi A, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med 2001;344(10):732–738
- Kamisawa T, Funata N, Hayashi Y, et al. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol 2003;38(10):982–984.
- Zen Y, Harada K, Sasaki M, et al. IgG4-related sclerosing cholangitis with and without hepatic inflammatory pseudotumor, and sclerosing pancreatitis-associated sclerosing cholangitis: do they belong to a spectrum of sclerosing pancreatitis? Am J Surg Pathol 2004;28(9):1193–1203
- Cheuk W, Yuen HK, Chu SY, Chiu EK, Lam LK, Chan JK. Lymphadenopathy of IgG4-related sclerosing disease. Am J Surg Pathol 2008;32(5):671–68
Dr. Jai Shilpa.
Consultant Radiologist.
Manipal Hospital Radiology Group (MHRG)
Manipal Hospital, Bengaluru.
Dr. Mayank M Rangari
Fellow in Radiology
Manipal Hospital Radiology Group (MHRG)
Manipal Hospital, Bengaluru.