A 48-year-old man with abdominal pain and constitutional syndrome with weight loss in the past 4 weeks
A 48-year-old man with abdominal pain and constitutional syndrome with weight loss in the past 4 weeks. Physical examination revealed diffuse abdominal pain without peritoneal irritation and a hard non-mobile
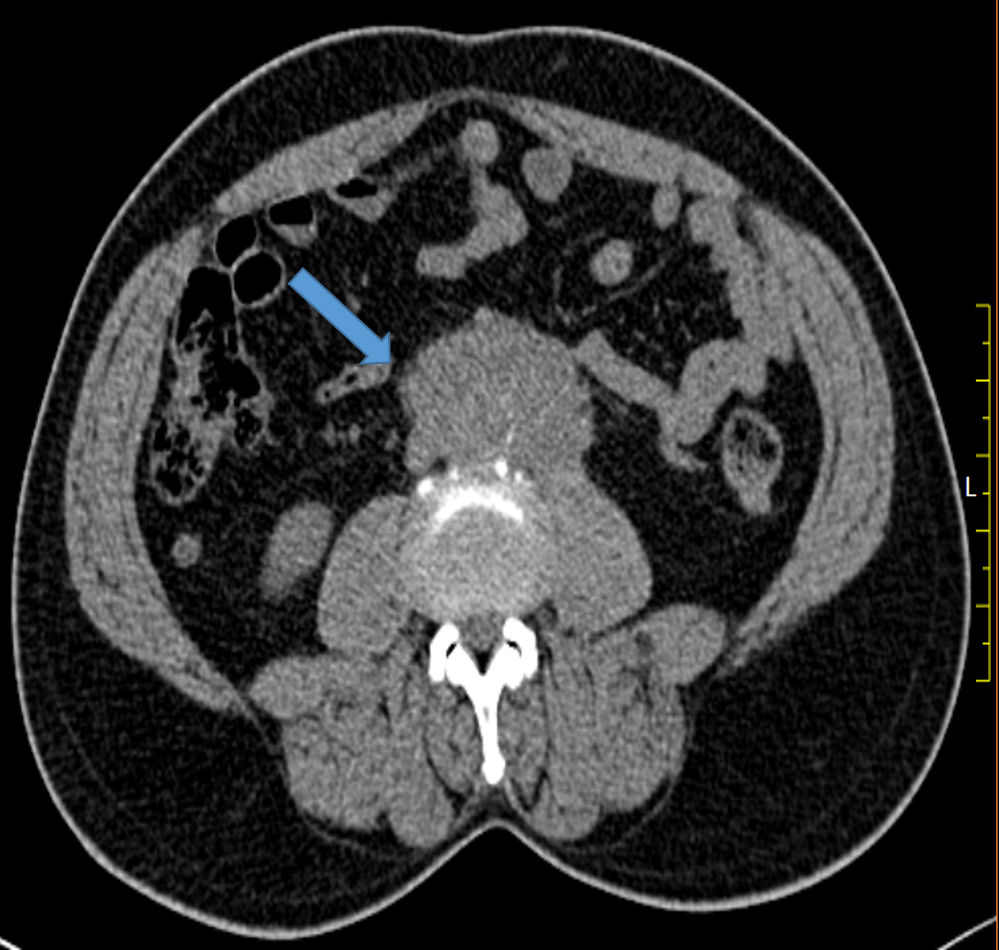
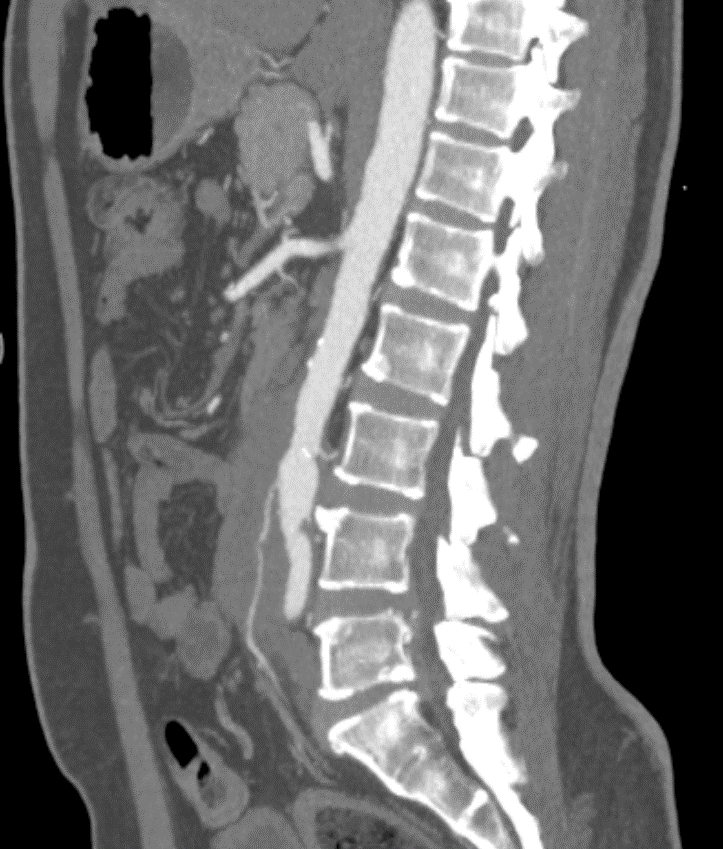
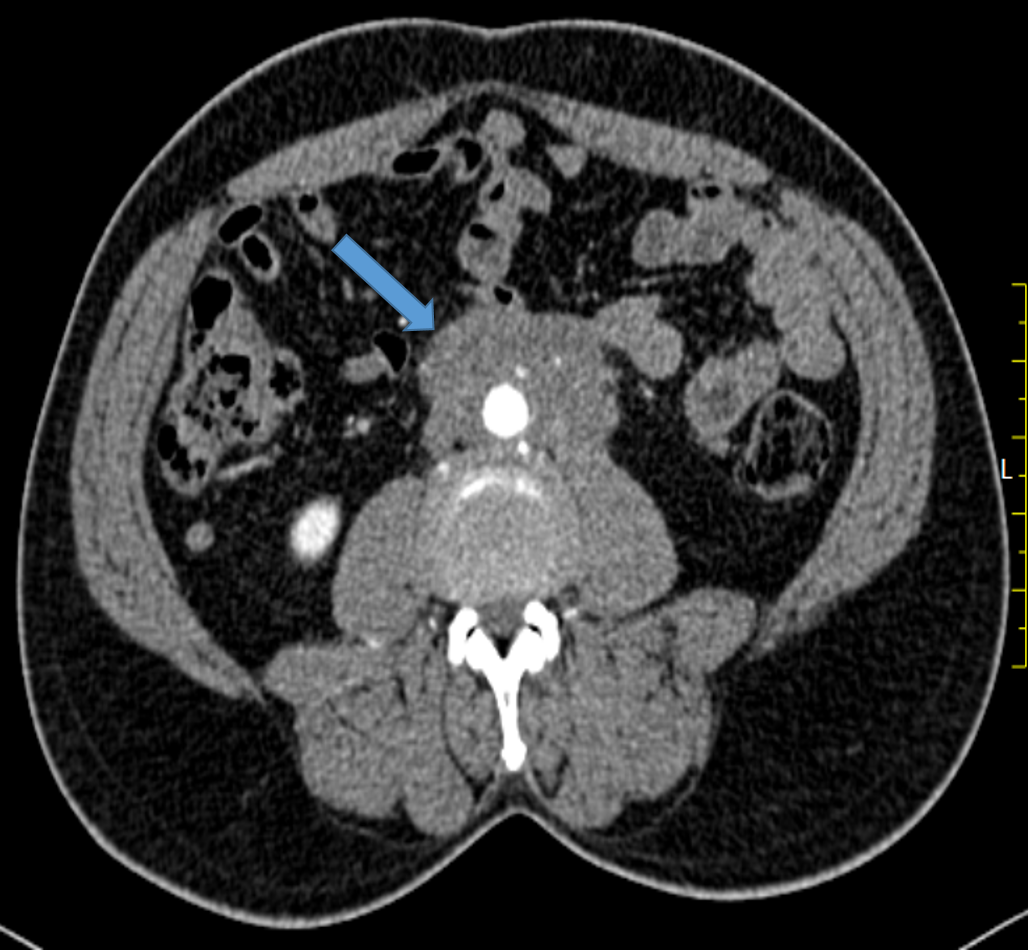
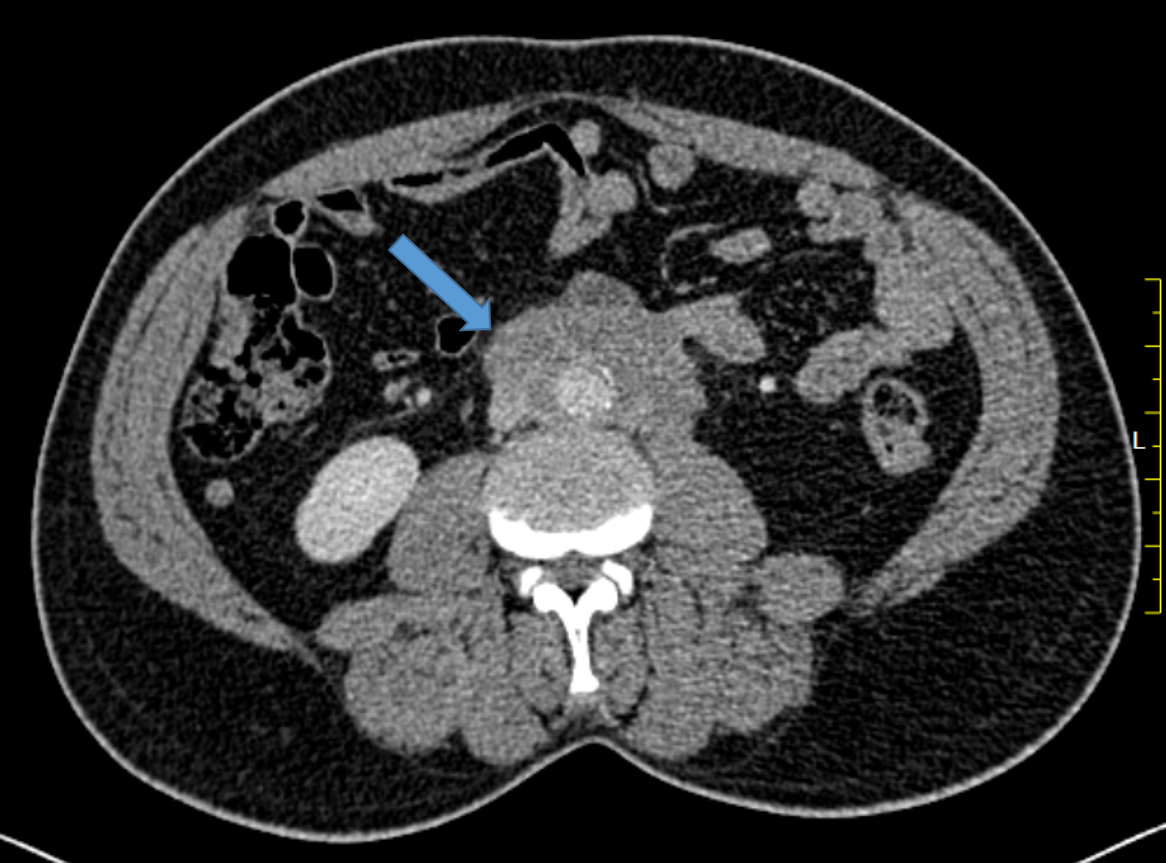
A : Ill-defined plaque like mild heterogeneously enhancing soft tissue density lesion in infra renal retroperitoneum completely encasing infra renal abdominal aorta extending up to its bifurcation. No significant elevation of the aorta or IVC seen.
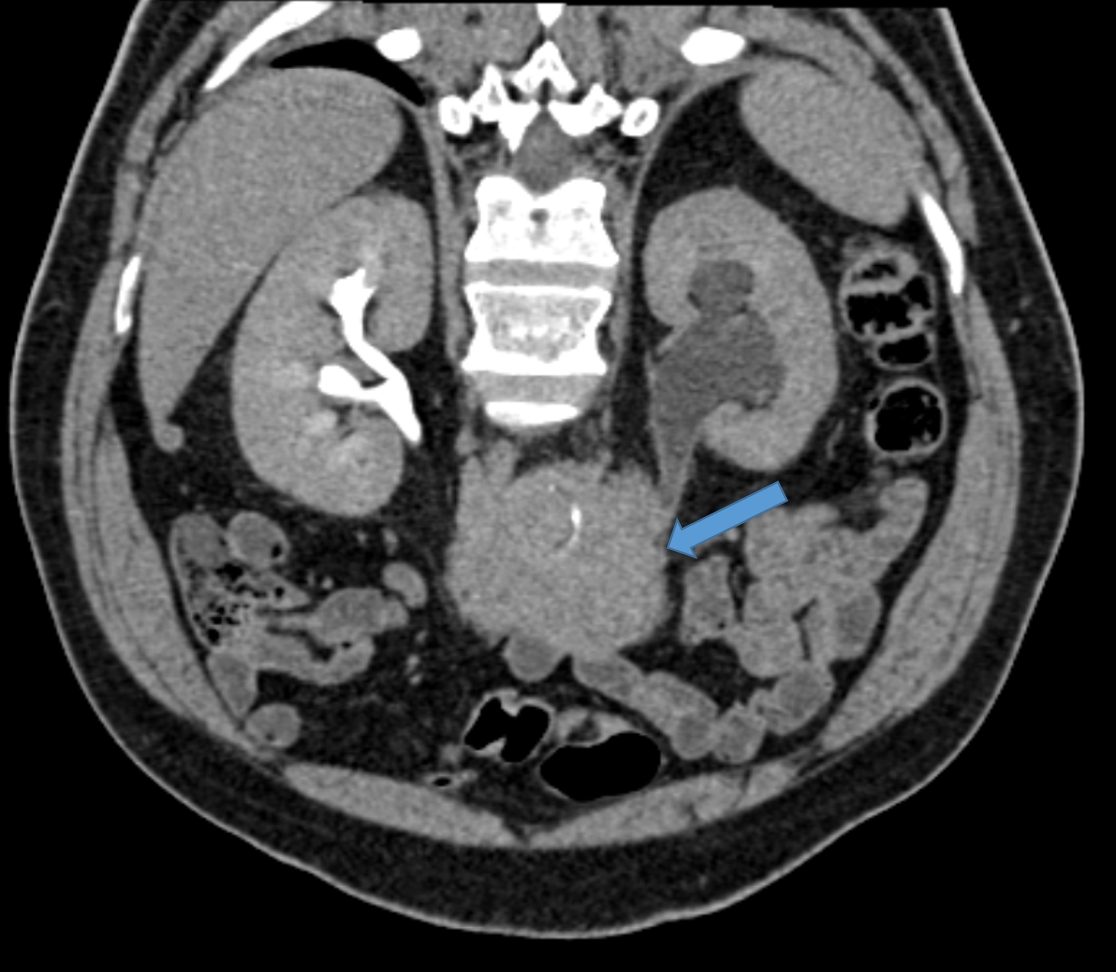
B : The lesion is causing complete encasement of IMA and partial encasement of IVC without luminal narrowing
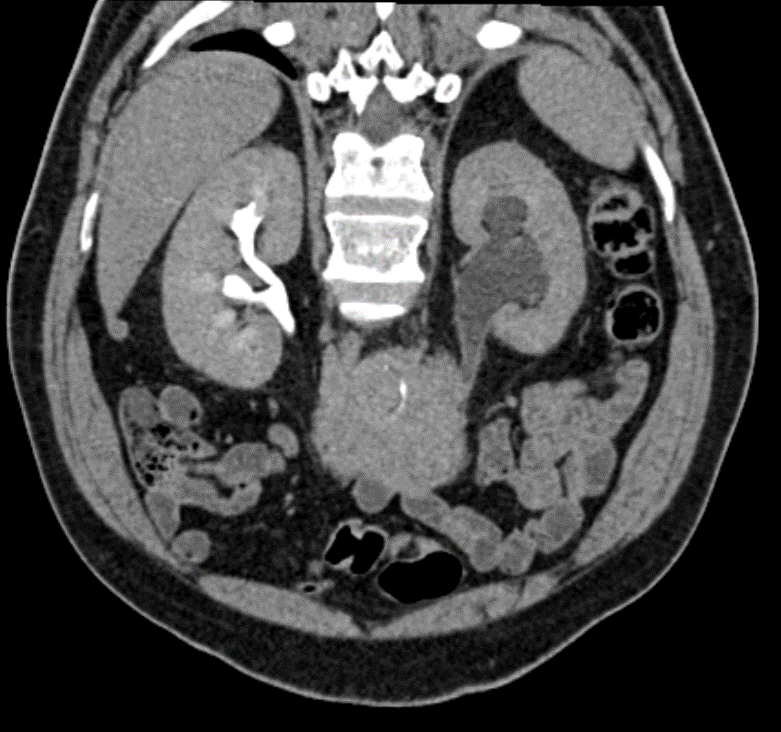
C : The lesion completely encases left mid ureter with resultant proximal moderate hydroureteronephrosis. No evident involvement of the right ureter. Left kidney shows poor contrast enhancement with excretion on delayed phase.
Discussion:
- RPF is a rare condition in which a fibroinflammatory tissue appears surrounding the abdominal aorta – periaortitis (mainly the infrarenal aorta), the iliac arteries and the inferior vena cava.
- The lesion can spread to adjacent organs, frequently with ureteral involvement, which can lead to renal failure.
- The disease is part of a spectrum of entities that have a common pathogenic process consisting of an inflammatory response to advanced atherosclerosis, combined with autoimmunologic factors:
- idiopathic retroperitoneal fibrosis
- perianeurysmal retroperitoneal fibrosis
- isolated periaortitis: corresponds to a non-aneurysmal form of chronic periaortitis
- inflammatory abdominal aortic aneurysm
CLINICAL PRESENTATION:
- Patients may present with systemic symptoms such as mild fever and malaise due to an ongoing inflammatory process.
- Sometimes patients present with flank or back pain which is not position-dependent and has a transient relief with oral non-steroidal anti-inflammatory drugs .
- If there is the involvement of the ureters, colicky ureteric pain may be present.
DIANGNOSTIC APPROACH:
- Imaging diagnostics in IBDI involve ultrasonography of the abdominal cavity, cholangiography, endoscopic retrograde cholangiopancreatography (ERCP), computed tomography, and magnetic resonance-cholangiography.
- Magnetic resonance cholangiography is a sensitive (85%-100%) and non-invasive imaging modality for the biliary tract. Currently, it is the “gold standard” in preoperative diagnosis of IBDI in patients qualifying for surgical reconstruction
RADIOGRAPHIC FEATURES:
- Contrast-enhancing fibrosis encases the retroperitoneal structures causing ureteric and vascular obstruction and displacement.
- Displacement of the aorta and IVC anteriorly away from the vertebral bodies are suggestive of malignant etiology.
- Invasion and disruption of bone and/or soft tissue structures suggests an aggressive process – infection or malignancy.
- Multiple subcentimeter lymph nodes are frequently seen in non-malignant RPF, probably reactive secondary to the disease process, and should not be confused for malignancy.
- MDCT and magnetic resonance imaging (MRI) are essential tools in the non-invasive diagnostic work-up as they can assess the location, morphology and extent of the lesion as well as the involvement of adjacent organs. Besides, they can detect associated diseases or the cause in case of secondary RPF.
CT
- In early or active stages, variable enhancement can be seen with intravenous contrast while no enhancement may be seen in the quiescent disease.
MRI
- MRI has been reported to be as sensitive as CT in its assessment of retroperitoneal fibrosis with the added advantage of high contrast resolution between closely apposed retroperitoneal structures.
- It can evaluate the urinary tracts using fast T2 weighted spin-echo sequences without requiring intravenous contrast in patients with impaired renal function.
- The soft tissue mass is usually dark on T1W and T2W unless there is an active inflammation whereby the T2W images can be hyperintense.
Nuclear medicine – FDG-PET
- Uptake will be seen in active inflammation and absent in metabolically inactive disease.
- A biopsy is usually obtained to con?rm the diagnosis.
- Corticosteroids are usually the first line of treatment for patients. The lesion usually responds to steroid therapy although immunosuppressive therapy can also be used.
- Imaging techniques can be used to assess response to treatment.
Imaging differentials:
- retroperitoneal lymphoma: non-lymphomatous RPF is often seen centered at L4/5 level; if the disease is centered cranially to L4/5, consider lymphoma along with floating aorta sign.
- retroperitoneal Erdheim-Chester disease.
- retroperitoneal extramedullaryhematopoiesis(rare).
References
- Martínez-de-Alegría A, Baleato-González S, García-Figueiras R, Bermúdez-Naveira A, Abdulkader-Nallib I, Díaz-Peromingo A, et al (2015) IgG4-related Disease from Head to Toe. Radiographics 35(7):2007-25 (PMID: 26473450)
- Hedgire SS; McDermott S, Borczuk D, Elmi A, Saini S, Harisinghani MG (2013) The spectrum of IgG4-related disease in the abdomen and pelvis. AJR Am J Roentgenol. 201(1):14-22 (PMID: 23789654)
- Ardila-Suarez O, Abril A, Gómez-Puerta JA (2017) IgG4-related Disease: A Concise Review of the Current Literature. Reumatología Clínica (English Edition), 13(3):160-166 (PMID: 27329319)
- Rossi GM, Rocco R, Accorsi Buttini E, Marvisi C, Vaglio A (2017) Idiopathic retroperitoneal fibrosis and its overlap with IgG4-related disease. Intern Emerg Med 12, 287–299 (PMID: 28070877)
- Lian L, Wang C, Tian J (2016) IgG4-related retroperitoneal ?brosis: a newly characterized disease. Int J Rheum Dis 19(11):1049-1055 (PMID: 27125330)
- Caiafa RO, Vinuesa AS, Izquierdo RS, Brufau BP, Ayuso Colella JR, Molina CN (2013) Retroperitoneal fibrosis: role of imaging in diagnosis and follow-up. Radiographics 33(2):535-52 (PMID: 23479712)
- Cohan RH, Shampain KL, Francis IR, Davenport MS, Stuart Wolf J, Marder W, et al (2018) Imaging appearance of fibrosing diseases of the retroperitoneum: can a definitive diagnosis be made?. Abdom Radiol 43(5):1204-1214 (PMID: 28849414)
Dr. JAISHILPA
Senior Consultant Radiologist
Manipal Hospital, Yeshwanthpur, Bengaluru.
Dr. VAIBHAV BHANDARI
Senior resident, Radiologist
Manipal Hospital, Yeshwanthpur, Bengaluru.